[Author: Laura Cowen]
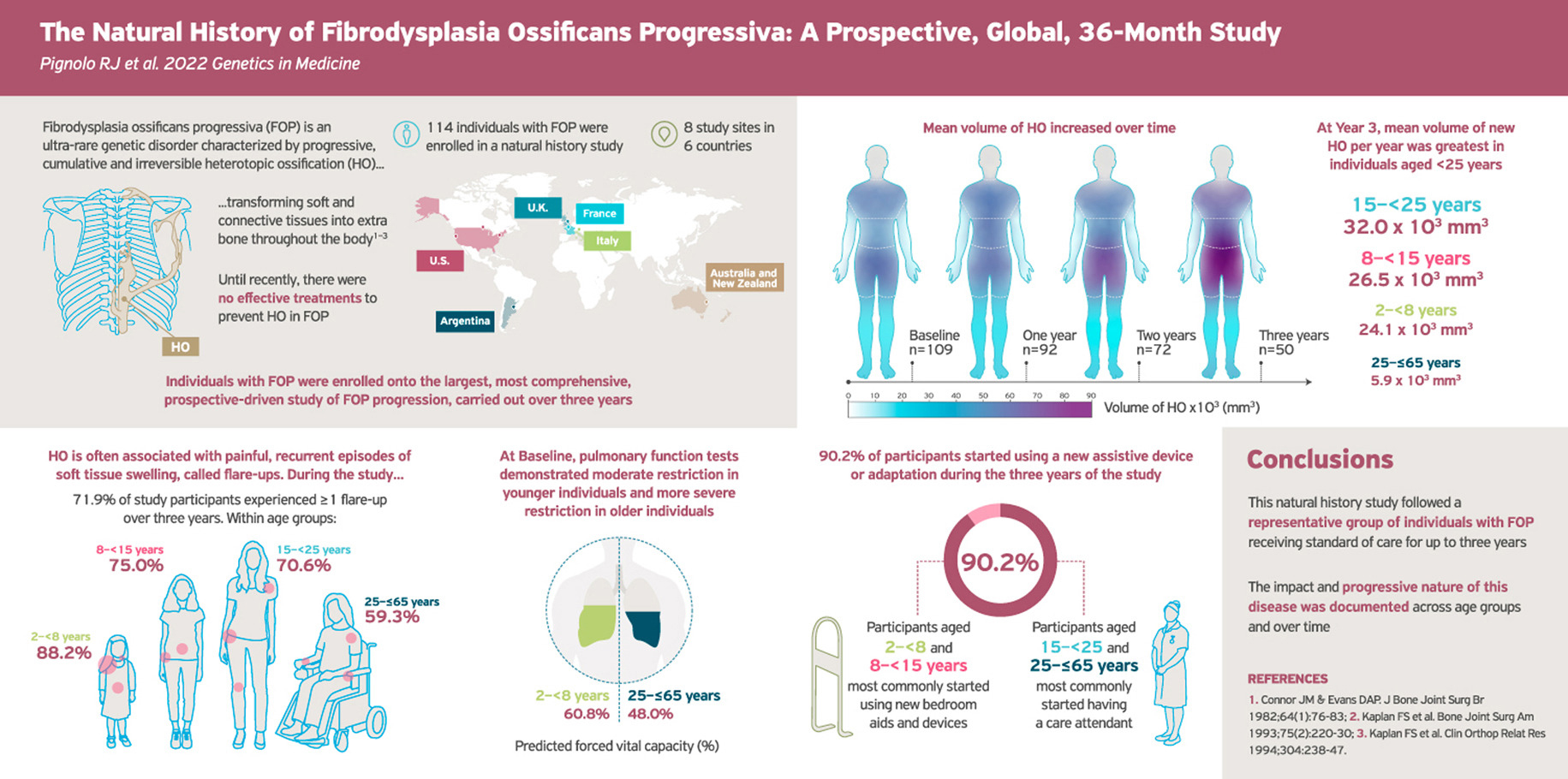
An international, 3-year study of people with fibrodysplasia ossificans progressive (FOP) has mapped the natural history of the disease and shown that the greatest levels of progression occur during childhood and early adulthood.
Robert Pignolo (Mayo Clinic, Rochester, Minnesota, USA) and co-authors say their findings “will facilitate the evaluation of meaningful end points in the development of new therapeutics, which are critically needed for individuals with FOP.”
The study included 114 individuals (54% male) aged 65 years and younger (median 15 years) with classical ACVR1R206H variant FOP, of whom 33 completed the full 3 years of follow-up. The main reason for discontinuation was subsequent enrollment in an interventional study (58%).
The mean follow-up duration was 26.8 months and during this time 71.9% of individuals reported 229 flare-ups, most commonly in the upper back (17.9%), hip (14.8%), and shoulder (10.9%).
In all, 52 flare ups in 40 (35.1%) participants were imaged by low-dose computed tomography (CT) and/or x-ray scans at the flare-up site on the day the individual presented with a flare-up or within 14 days of the flare-up/suspected flare-up, and then 84 days later to measure the extent of heterotropic ossification (HO) at the flare-up site. Participants in the youngest age group (2–<8 years) were almost twice as likely to have imaging at flare up as those in the oldest age group (25–65 years), at a rate of 47.1% versus 25.9%.
The researchers report that HO was present at the flare-up site in 71.2% of imaged flare-ups on day 1. At day 84, 26.9% had new HO at the flare-up site, with a mean new HO volume of 28.8×103 mm3.
Mean baseline low-dose whole-body (excluding head) CT HO volume was 306.1×103 mm3 overall but increased with age, from 68.8×103 mm3 in the youngest group to 595.0×103 mm3 in the oldest.
Participants aged 15 to 24 years had the highest mean annualized volume of new HO, at 41.5×103 mm3/year followed by those aged 8 to 14 years and aged 2 to 7 years, at 21.9 and 18.6×103 mm3/year, respectively. The oldest participants had the lowest annualized new HO volume, at a mean of 4.6×103 mm3/year.
New HO was predominantly detected in the upper- and mid-torso regions of participants below 15 years of age and predominantly in the hip and lower-leg regions in aged 15 to 24 years. Older participants had relatively small volumes of new HO across all body regions during the study. In spite of this, approximately 70% continued to accumulate new HO.
“With increasing age, smaller changes in HO volumes may be attributable to multiple factors, including reduced soft tissue availability for conversion to HO and a decrease in the initiation of new HO lesions,” write Pignolo and co-authors in Genetics in Medicine.
The researchers also looked at changes in functional measures but observed only small increases in the Cumulative Analogue Joint Involvement Scale (CAJIS) and the FOP Physical Function Questionnaire (FOP-PFQ) during the study.
Specifically, each 100.0×103 mm3 increase in whole-body CT HO volume was associated with a significant 1.1-point increase in CAJIS total score and a significant 4.0% increase in FOP-PFQ percentage of worst total score.
Although the changes in these outcomes were limited, nearly all (90.2%) participants began using new aids, assistive devices, and adaptations (AADAs) during follow-up. Younger participants (<15 years) most commonly started using new bedroom aids and devices, while their older counterparts most commonly started having a care attendant.
Analysis of cardiopulmonary function showed that the youngest study participants (2-<8 years) had the highest mean percent predicted forced vital capacity (FVC), at 60.8%. This fell with age before reaching a plateau at around 48% in the early 20s, which the investigators say “is consistent with worsening restrictive lung disease in individuals with FOP during their early to late teenage years and early 20s, at which point most individuals have clinically significant, but stable, restrictive chest wall disease.”
Most (79.8%) patients initiated a new medication during follow-up, typically glucocorticoids (32.5%) or non-steroidal anti-inflammatory drugs (31.6%), and the researchers note that “[a] disproportionately higher percentage of individuals aged 2 to <8 years initiated corticosteroids for systemic use than the other age groups.”
Pignolo et al. say that their study is “the largest, most comprehensive, prospective [natural history study] of FOP to date,” adding that it is the first “to carefully assess flare-up characteristics and the association of new HO with functional end points.”
They conclude: “Given the size and representability of the data set relative to the known world-wide population of people with FOP (approximately 15% of all known individuals were included), data obtained from this NHS will be instrumental in the design and execution of interventional trials of potential therapeutics in FOP.”